COVID-19 nasal vaccines – the way forward?

Despite 98.1% of adults in the UK having antibodies to COVID-19, the number of cases seems to be increasing again. With the appearance of the new Omicron variant, it might be time for the introduction of a new protective measure to boost our immunity – nasal vaccines.
As a respiratory virus, SARS-CoV-2 enters the body through the airways, initiates infection in the mucous membranes of the nose and throat and is shed in respiratory droplets through coughing and sneezing. Stimulating an immune response in those areas, therefore, may kill those pathogens and prevent their spread into the lungs.
It is thought that this new form of COVID-19 vaccine could provide a stronger barrier from infection than classic injected vaccines. Most importantly, it could drastically reduce the transmission of COVID-19.
How do nasal vaccines work?
Nasal vaccines are not a new idea. FluMist, a nasal flu vaccine, has been approved for use since 2003 and is recommended by the Centre for Disease Control and Prevention (CDC).
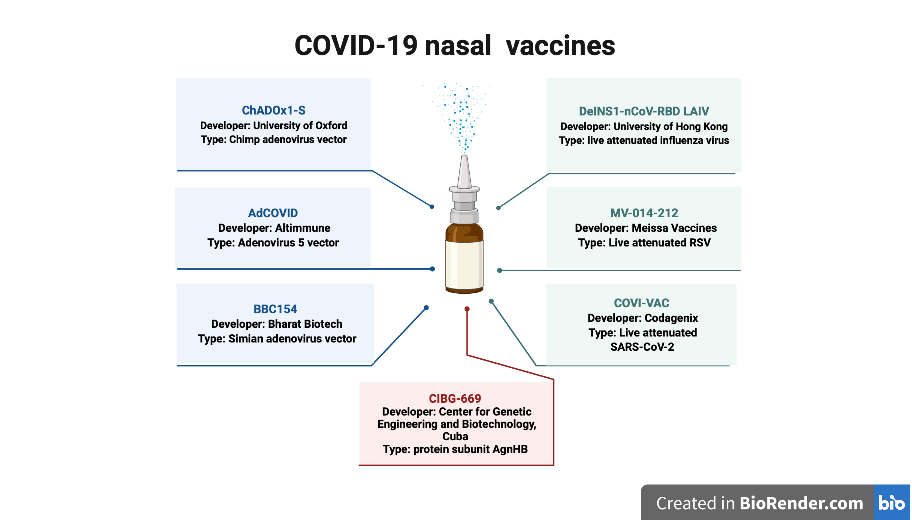
For COVID-19, there are currently seven nasal spray vaccines in clinical trial. Six of these contain either live-attenuated viruses – weakened versions of the virus which should not cause disease in people with healthy immune systems – or virus-vectored vaccines. These direct our own cells to create antigens. These have both been shown to be effective at triggering an immune response.
In particular, they activate CD8+ T cells, which directly kill infected cells and are vital to inhibiting viral replication and clearing the infection from the body. Several of these T cells also differentiate into memory cells, which can be rapidly reactivated upon subsequent infection with the same virus. In short, these vaccines provide strong immunity to COVID-19.
The other intranasal vaccine being developed contains a protein subunit, which has been shown to cause weak activation of CD8+ T cells.
All these needle-free vaccines deliver antigens to the site of infection – the respiratory tract – and produce a robust local immune response in the mucosal tissues of the tract. Intramuscular injections, on the other hand, only stimulate a weak immune response in the mucosa of the nose and throat.
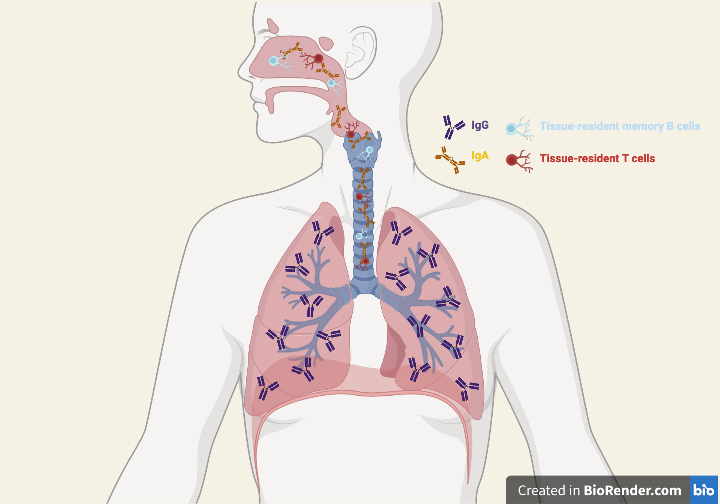
Vaccines injected into the arm predominantly activate immunoglobulin G (IgG), a type of antibody that is found in the lower lung and fights viral infection there. IgG can be found in the upper respiratory tract and the nasal passages, but high numbers of these antibodies are needed to protect these sites from infection.
A study on the role of different antibodies in anti-influenza virus immune responses in mice showed that the concentration of IgG required to reduce viral shedding was 3 times higher than that required of immunoglobulin A (IgA). In fact, only IgA was found to prevent infection of the upper respiratory tract, whereas IgG was required to block lung infection. It follows then, that IgA may be vital to reducing the spread of the virus from the respiratory tract of people infected with SARS-CoV-2.
Why are they useful?
We know that nasal infection and vaccination triggers the production of IgA antibodies, which are released into the airways to neutralise the SARS-CoV-2 virus. Moreover, the IgA response induced is much greater with intranasal vaccines than with intramuscular injections.
These antibodies are primarily found in the upper airways and nasal passages; consequently, these vaccines produce a much stronger immune response at the sites of initial infection. Additionally, nasal vaccinations produce immune cells which migrate to the mucosal linings of the respiratory tract, where they persist to release antibodies or become memory cells.
These tissue-resident memory cells provide a first line of defence against infection and respond more quickly than systemic memory cells. This allows them to clear the virus promptly, reducing its replication and shedding.
Both the superior IgA response and the resident memory cells in the respiratory mucosa provide solid evidence that nasal vaccines could successfully inhibit transmission of COVID-19.
The end of intramuscular injections?
For all their benefits, nasal vaccines are not a perfect solution to COVID-19. Antibody responses in the mucosal linings often have short durations and lung-specific memory cells do not tend to persist for long periods of time. Conversely, intramuscular injections produce circulating memory cells which self-renew and therefore stay in the body for a long time.
Furthermore, the immune response generated by intranasal vaccination is strong in the nose and throat but may be less effective throughout the rest of the body. There is also the risk of infection and illness with the delivery of live attenuated viruses, which is absent from the mRNA vaccines currently being used to prevent COVID-19.
These factors indicate that nasal vaccines may be best suited as a booster shot after giving intramuscular injection, which would result in both a local and systemic immune response.
Although the extent of their future use is uncertain, nasal vaccines have the potential to be an effective and easy protective measure against COVID-19, with the added benefit of not involving needles. The COVID-19 nasal vaccines are currently in the early stages of clinical trials, and it may be some time before they’re able to enter common usage.
However, in this period of rapid biomedical development, it doesn’t seem too far-fetched to imagine a world in which we all have our COVID-19 nasal sprays to hand.